Developing an AI Model That Relies on Mobile Health Devices to Track Heart Activity
DOI:
https://doi.org/10.51173/jt.v6i3.2576Keywords:
AI, Python Programming, TensorFlow, Google Colab, Simulation DataAbstract
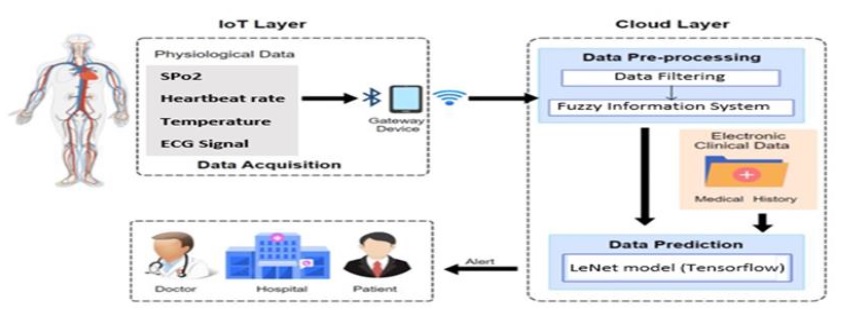
Heart disease lies among the top causes of death worldwide and accounts for a large number of deaths annually. Researchers are using artificial intelligence as a potent tool to construct cutting-edge healthcare applications in an effort to address this problem for the detection and avoidance of heart disease. This article presents the design and development of an artificial intelligence model using Python, TensorFlow, and Google Colab resources. Trained son simulation data with an 80:20 train/validation split and employing the Adam optimizer over 50 epochs, the model achieved an impressive 95% accuracy. Utilizing input data sumlation data from temperature, SPo2, heart rate and ECG signal the AI model predicts the individual's health state with a confidence level of 95%.
Downloads
References
K. W. Johnson et al., “Artificial intelligence in cardiology,” Journal of the American College of Cardiology, vol. 71, no. 23, pp. 2668–2679, Jun. 2018, doi: 10.1016/j.jacc.2018.03.521.
A. Lin, M. Kolossváry, I. Išgum, P. Maurovich‐Horvat, P. J. Slomka, and D. Dey, “Artificial intelligence: improving the efficiency of cardiovascular imaging,” Expert Review of Medical Devices, vol. 17, no. 6, pp. 565–577, Jun. 2020, doi: 10.1080/17434440.2020.1777855.
S. Azzi, S. Gagnon, A. Ramírez, and G. Richards, “Healthcare Applications of Artificial Intelligence and Analytics: A review and Proposed framework,” Applied Sciences, vol. 10, no. 18, p. 6553, Sep. 2020, doi: 10.3390/app10186553.
M. Martínez‐Sellés and M. Marina-Breysse, “Current and future use of artificial intelligence in electrocardiography,” Journal of Cardiovascular Development and Disease, vol. 10, no. 4, p. 175, Apr. 2023, doi: 10.3390/jcdd10040175..
D. Lee and S. N. Yoon, “Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and challenges,” International Journal of Environmental Research and Public Health/International Journal of Environmental Research and Public Health, vol. 18, no. 1, p. 271, Jan. 2021, doi: 10.3390/ijerph18010271
A. J. A. Majumder, Y. ElSaadany, R. A. Young, and Ucci, “An energy efficient wearable smart IoT system to predict cardiac arrest,” Advances in Human-computer Interaction, vol. 2019, pp. 1–21, 2019, doi: 10.1155/2019/1507465.
R. Katarya and P. Srinivas, "Predicting Heart Disease at Early Stages using Machine Learning: A Survey," 2020 International Conference on Electronics and Sustainable Communication Systems (ICESC), Coimbatore, India, 2020, pp. 302-305, doi: 10.1109/ICESC48915.2020.9155586.
G. Briganti and O. L. Moine, “Artificial intelligence in Medicine: Today and tomorrow,” Frontiers in Medicine, vol. 7, Feb. 2020, doi: 10.3389/fmed.2020.00027.
G. Karimian, E. Petelos, and S. M. a. A. Evers, “The ethical issues of the application of artificial intelligence in healthcare: a systematic scoping review,” AI And Ethics, vol. 2, no. 4, pp. 539–551, Mar. 2022, doi: 10.1007/s43681-021-00131-7.
J. M. Pevnick, K. Birkeland, R. Zimmer, Y. Elad, and I. Kedan, “Wearable technology for cardiology: An update and framework for the future,” Trends in Cardiovascular Medicine, vol. 28, no. 2, pp. 144–150, Feb. 2018, doi: 10.1016/j.tcm.2017.08.003.
A. T. Shumba et al., “Wearable Technologies and AI at the far Edge for Chronic Heart Failure Prevention and Management: A Systematic Review and Prospects,” Sensors, vol. 23, no. 15, p. 6896, Aug. 2023, doi: 10.3390/s23156896.
Y. -J. Lin et al., "Artificial Intelligence of Things Wearable System for Cardiac Disease Detection," 2019 IEEE International Conference on Artificial Intelligence Circuits and Systems (AICAS), Hsinchu, Taiwan, 2019, pp. 67-70, doi: 10.1109/AICAS.2019.8771630.
A. Šećkanović et al., "Review of Artificial Intelligence Application in Cardiology," 2020 9th Mediterranean Conference on Embedded Computing (MECO), Budva, Montenegro, 2020, pp. 1-5, doi: 10.1109/MECO49872.2020.9134333.
A. Gearhart, S. Gaffar, and A. Chang, “A primer on artificial intelligence for the paediatric cardiologist,” Cardiology in the Young, vol. 30, no. 7, pp. 934–945, Jun. 2020, doi: 10.1017/s1047951120001493.
R. Vashistha, A. K. Dangi, A. Kumar, D. Chhabra, and P. Shukla, “Futuristic biosensors for cardiac health care: an artificial intelligence approach,” 3 Biotech, vol. 8, no. 8, Aug. 2018, doi: 10.1007/s13205-018-1368-y.
Y. Yang, J. Zhang, G. Zang, and J. Pu, “The primary use of artificial intelligence in cardiovascular diseases: what kind of potential role does artificial intelligence play in future medicine?,” PubMed, vol. 16, no. 8, pp. 585–591, Aug. 2019, doi: 10.11909/j.issn.1671-5411.2019.08.010.
P. Bächtiger et al., “Artificial intelligence, data sensors and interconnectivity: future opportunities for heart failure,” Cardiac Failure Review, vol. 6, May 2020, doi: 10.15420/cfr.2019.14.
C. Krittanawong et al., “Integration of novel monitoring devices with machine learning technology for scalable cardiovascular management,” Nature Reviews. Cardiology, vol. 18, no. 2, pp. 75–91, Oct. 2020, doi: 10.1038/s41569-020-00445-9.
A. Javaid et al., “Medicine 2032: The future of cardiovascular disease prevention with machine learning and digital health technology,” American Journal of Preventive Cardiology, vol. 12, p. 100379, Dec. 2022, doi: 10.1016/j.ajpc.2022.100379.
G. Y. H. Lip, A. Genaidy, and C. Estes, “Cardiovascular disease (CVD) outcomes and associated risk factors in a medicare population without prior CVD history: an analysis using statistical and machine learning algorithms,” Internal and Emergency Medicine, vol. 18, no. 5, pp. 1373–1383, Jun. 2023, doi: 10.1007/s11739-023-03297-6.
L. Neri et al., “Electrocardiogram Monitoring wearable devices and Artificial-Intelligence-Enabled Diagnostic Capabilities: A review,” Sensors, vol. 23, no. 10, p. 4805, May 2023, doi: 10.3390/s23104805.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Hamdan H. Shehab, Fadi Al-Turjman

This work is licensed under a Creative Commons Attribution 4.0 International License.