Practices Regarding Human Papillomavirus and Cervical Cancer in A Sample of Paramedical Staff in Al- Najaf Governorate, Iraq
DOI:
https://doi.org/10.51173/jt.v4i33.613Keywords:
Human papilloma virus, Cervical cancer, Practice, Paramedical staff, Najaf governorateAbstract
The papillomaviridae viral family includes HPV. When it comes to female sexually transmitted diseases, the genital tract is the primary site of infection for genital type HPVs, which are further divided into high- and low-risk subgroups depending on the likelihood that they will cause cancer of the genital tract. High-risk HPV strains 16 and 18 cause cervical cancer. Sexual contact or skin-to-skin contact is the primary mode of transmission of HPV.
To assess the degree of Practice among a sample of paramedical workers concerning the Human Papillomavirus and Cervical Cancer.
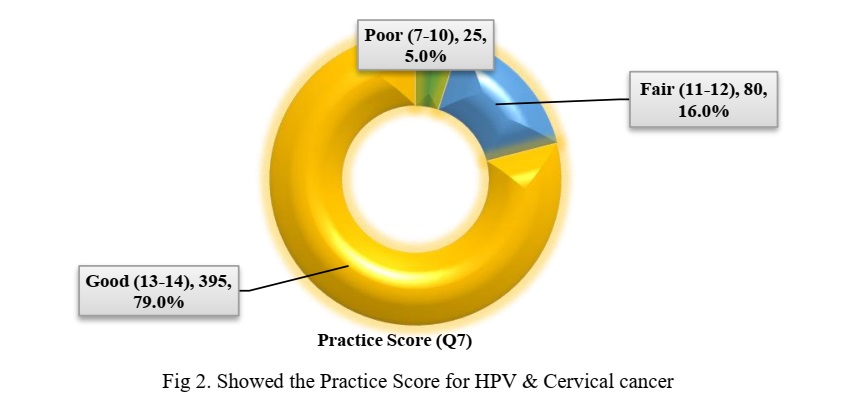
Five hospitals and 25 primary health care centers in the Al-Najaf governorate were studied in this cross-sectional observational descriptive cross-sectional research. Starting on December 19th, 2021 and concluding on April 18th, 2022, data was gathered for four months. According to the results of the present research, which included (five hundred) Paramedical employees aged 20-59 years, the age group with the largest proportion (66.4%) was that of 20-29 years. Whereas, in terms of gender, the largest proportion of women (64.6 percent). Almost all paramedics work in urban areas. In addition, almost half of the participants came from medical institutions, accounting for 51.6 percent of the total, while just 2.4 percent were graduates of secondary schools. Only 2.4% of the paramedical staff had any kind of education or training on HPV or cervical cancer. Excellent practice evaluations for the Human Papillomavirus and cervical cancer were much higher among paramedical providers (79 percent). Most of the paramedics who were evaluated for their practices addressing cervical cancer and the human papillomavirus (HPV) received good grades. Health authorities, social groupings, and non-governmental organizations should work together to communicate information about the human papillomavirus and cervical cancer to the general population. In order to educate and sensitize medical professionals about HPV screening technologies and the most current screening and treatment guidelines, conduct educational initiatives.
Downloads
References
Wang, R., Pan, W., Jin, L., Huang, W., Li, Y., Wu, D., ... & Liao, S. (2020). Human papillomavirus vaccine against cervical cancer: Opportunity and challenge. Cancer letters, 471, 88-102.
Jalil, A. T., Kadhum, W. R., Faryad Khan, M. U., Karevskiy, A., Hanan, Z. K., Suksatan, W., ... & Abdullah, M. M. (2021). Cancer stages and demographical study of HPV16 in gene L2 isolated from cervical cancer in Dhi-Qar province, Iraq. Applied Nanoscience, 1-7.
Gravitt, P. E., & Winer, R. L. (2017). Natural history of HPV infection across the lifespan: role of viral latency. Viruses, 9(10), 267.
Kaufman, H. W., Alagia, D. P., Chen, Z., Onisko, A., & Austin, R. M. (2021). Cotesting in Cervical Cancer Screening. American Journal of Clinical Pathology, 155(1), 150-155.
Hassan, H. E., Masaud, H., Mohammed, R., & Ramadan, S. (2021). Self-knowledge and body image among cervical cancer survivors women in northern upper Egypt. Journal of Applied Health Sciences and Medicine, 1(1), 1-12.
Ali, S. (2018). Evidence based strategies to establish population-based cervical cancer screening in Kirkuk, Iraq (Doctoral dissertation, University of Plymouth).
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 71(3), 209-249.
Fadiel, R. N., Chiad, I. A., & Kadhum, S. A. Knowledge Regarding Nosocomial Infection Among A Sample Of Paramedical Staff In Al-Najaf Governorate. Turkish Journal of Physiotherapy and Rehabilitation, 32, 3.
Idrees, F., Ahmad, S., & Rehman, A. (2022). Assessing Knowledge, Attitudes And Practices Towards Cervical Cancer Among Women In Rawalpindi–Pakistan. Palarch's Journal of Archaeology of Egypt/Egyptology, 19(2), 443-457.
Mehaboob, S. H., Nandini, T. U., Prameela, G., Sireesha, M., Narayana, G., & VeeraBadrappa, K. (2016). Knowledge, attitude & practices regarding cervical cancer awareness in women staff of secondary care referral hospital. I JI RI, 4, 106-112.
Singh, J., & Baliga, S. S. (2021). Knowledge regarding cervical cancer and HPV vaccine among medical students: a cross-sectional study. Clinical Epidemiology and Global Health, 9, 289-292.
Swarnapriya, K., Kavitha, D., & Reddy, G. M. M. (2016). Knowledge, attitude and practices regarding HPV vaccination among medical and para medical in students, India a cross sectional study. Asian Pacific Journal of Cancer Prevention, 16(18), 8473-8477.
Gebisa, T., Bala, E. T., & Deriba, B. S. (2022). Knowledge, Attitude, and Practice Toward Cervical Cancer Screening Among Women Attending Health Facilities in Central Ethiopia. Cancer Control, 29, 10732748221076680.
Najafi-Sharjabad, F., & Rayani, M. (2019). The relationship between knowledge, attitude and acceptance of Human Papilloma Virus (HPV) vaccination for cervical cancer prevention among students at Bushehr University of Medical Sciences, Iran. Journal of Research Development in Nursing and Midwifery, 16(2), 19-29
Majid, E., Shaikh, M. A., Qazi, O. A., Khan, S., Majeed, I., & Bano, K. (2022). Awareness, screening, Practices and attitudes of cervical cancer among doctors and nursing staff working at a tertiary care center. Journal of the Pakistan Medical Association.
Al-Sarray, A. A. M. Knowledge and Attitudes About the Human Papilloma Virus and Cervical Cancer Among a Sample of Paramedical Students in Baghdad Teaching Hospital. IJPQA 2019,10(1);186-192
Ebu, N. I., Abotsi-Foli, G. E., & Gakpo, D. F. (2021). Nurses’ and midwives’ knowledge, attitudes, and acceptance regarding human papillomavirus vaccination in Ghana: a cross-sectional study. BMC nursing, 20(1), 1-10.
Chellapandian, P., Myneni, S., Ravikumar, D., Padmanaban, P., James, K. M., Kunasekaran, V. M., . . . Balu, P. (2021). Knowledge on cervical cancer and perceived barriers to the uptake of HPV vaccination among health professionals. BMC Women's Health, 21(1), 1-8.
Chawla, P. C. (2014). Role of healthcare providers in patient education on HPV infection and cervical cancer prevention–A crosssectional study in public & private health centers of Delhi-NCR, India. Int J Latest Res Sci Technol, 3, 140-146.
Singh, E., Seth, S., Rani, V., & Srivastava, D. K. (2012). Awareness of cervical cancer screening among nursing staff in a tertiary institution of rural India. Journal of gynecologic oncology, 23(3), 141-146.
Almazrou, S., Saddik, B., & Jradi, H. (2020). Knowledge, attitudes, and practices of Saudi physicians regarding cervical cancer and the human papilloma virus vaccine. Journal of Infection and Public Health, 13(4), 584-590.
Winarto, H., Habiburrahman, M., Dorothea, M., Wijaya, A., Nuryanto, K. H., Kusuma, F., ... & Anggraeni, T. D. (2022). Knowledge, attitudes, and practices among Indonesian urban communities regarding HPV infection, cervical cancer, and HPV vaccination. PloS one, 17(5), e0266139.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Alaa Mehdi Salih, Atta Ah Mousa Al –Sarray

This work is licensed under a Creative Commons Attribution 4.0 International License.