Comorbidities among Patients with Epilepsy Attending Imam Al-Sadiq General Hospital in Babylon Governorate, Iraq
DOI:
https://doi.org/10.51173/jt.v4i33.607Keywords:
Epilepsy, Comorbidities, Prevalence, Cognitive, BabylonAbstract
People with epilepsy often have other health conditions. Epidemiological findings are an important source of information on the topic of epilepsy comorbidity. These investigations show that patients with epilepsy frequently suffer from co-occurring disorders, involving nearly all body systems.
This study aims to determine the frequency of comorbidities among epilepsy patients. Patient and method: a descriptive cross-sectional study conducted at Imam Al-Sadiq general hospital, included 225 participants collected from 10th January/2022 to 10th May/2022. The samples were collected under the supervision of a neurologist.
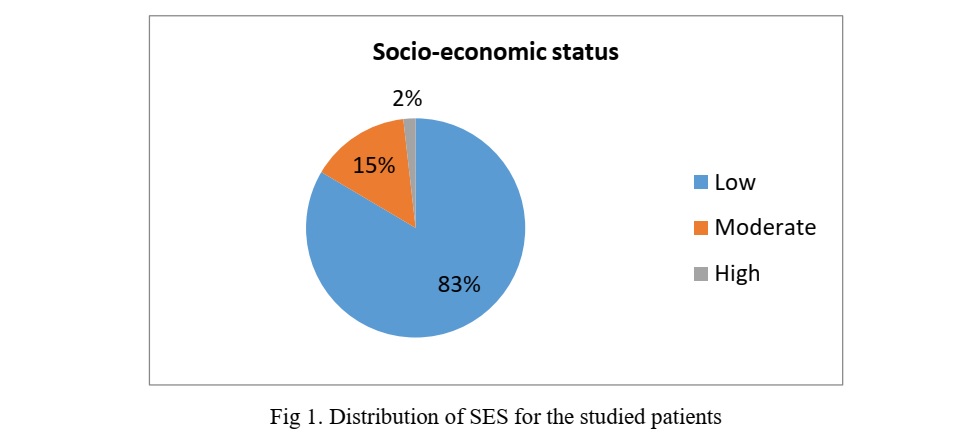
The mean age of epilepsy was 32.26 ± 13.94. 55.6% of the participants were males and 44.4% were females, the male to female ratio was 1.25:1. Vast majority (83.5%) of the studied samples had a low socio-economic status. prevalence of comorbidities among patients with epilepsy was high Among medical comorbidities, the highest percentage (56.9%) of participants were suffering from migraine. Among psychiatric comorbidities, 67.1% of them were suffered from anxiety and 61.9% with depression. 7.6% of patient were suffering from Dementia/ Alzheimer’s disease as cognitive comorbidities.
It found an increased risk for full spectrum of medical, psychiatric disorders. The most common medical comorbidities were migraines and musculoskeletal system disorders. more than half of participants were suffering from anxiety and depression, half of them with sleep disorders.
More comprehensive assessment with advanced diagnostic and treatment standards and treating not only the epilepsy but also any other present conditions.
Downloads
References
Muhigwa A, Preux PM, Gérard D, Marin B, Boumediène F, Ntamwira C, et al. Comorbidities of epilepsy in low and middle-income countries: systematic review and meta-analysis. Sci Rep. 2020;10(1):1–12
Sirven JI. Epilepsy: a spectrum disorder. Cold Spring Harb Perspect Med. 2015;5(9):a022848.
Seidenberg M, Pulsipher DT, Hermann B. Association of epilepsy and comorbid conditions. Future Neurol. 2009;4(5):663–8.
Keezer MR, Sisodiya SM, Sander JW. Comorbidities of epilepsy: Current concepts and future perspectives. Lancet Neurol [Internet]. 2016;15(1):106–15. Available from: http://dx.doi.org/10.1016/S1474-4422(15)00225-2.
Naydenov K, Petkov Y, Manchev I, Chengeliyska V, Komsiyska1 D. Comorbidity of epilepsy and mental disorders. Trakia J Sci. 2019;17(3):243–6.
Razak A, Mousawi A, Haydari APC of E and D in AHTH in HK/ I in 2018. Original Paper Comorbidity of Epilepsy and Depression in Al Husseini Teaching Hospital in Holy Kerbala / Iraq in 2018. 2020;13(1).
Jorge B, Rajesh, Carter S. These Guidelines are a Product of Critical Care Services Ontario ( CCSO ) and How to Use This Document For information about these Guidelines , please contact : Program of the Ontario Brain. 2020;2(March):52.
Kroenke K, Spitzer RL, Williams JBW. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Scott AJ, Sharpe L, Loomes M, Gandy M. Systematic review and meta-analysis of anxiety and depression in youth with epilepsy. J Pediatr Psychol. 2020;45(2):133–44.
Alsaadi T, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, Nasreddine W, et al. Depression and anxiety among patients with epilepsy and multiple sclerosis: UAE comparative study. Behav Neurol. 2015;2015:4.
Jafaar SA. Quality Of Life For Patients With Epilepsy In Baghdad City. kufa J Nurs Sci. 2014;4(2).
Shakir M, Al-Asadi JN. Quality of life and its determinants in people with epilepsy in Basrah, Iraq. Sultan Qaboos Univ Med J. 2012;12(4):449.
Hamed SA, Moussa EMM, Youssef AH, Abd ElHameed MA, NasrEldin E. Bone status in patients with epilepsy: relationship to markers of bone remodeling. Front Neurol. 2014;5:142.
Louay Hashim S, Mohammad Tawfik R. Migraine in epileptic patients epidemiology and clinical characteristics. 2006;
St. Germaine-Smith C, Liu M, Quan H, Wiebe S, Jette N. Development of an epilepsy-specific risk adjustment comorbidity index. Epilepsia. 2011;52(12):2161–7.
A. Staniszewska, A. Mąka, U. Religioni, and D. Olejniczak, “Sleep disturbances among patients with epilepsy,” Neuropsychiatr. Dis. Treat., vol. 13, p. 1797, 2017.
Tegegne MT, Mossie TB, Awoke AA, Assaye AM, Gebrie BT, Eshetu DA. Depression and anxiety disorder among epileptic people at amanuel specialized mental hospital, Addis Ababa, Ethiopia. BMC Psychiatry. 2015;15(1):1–7.
Clancy MJ, Clarke MC, Connor DJ, Cannon M, Cotter DR. The prevalence of psychosis in epilepsy; a systematic review and meta-analysis. BMC Psychiatry. 2014;14(1):1–9.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Bilal Hadi Jawad, Khadija Shaban Hassan, Wahab Razzaq Ebdan

This work is licensed under a Creative Commons Attribution 4.0 International License.