Phenotypic Resistance of (MRSA) Clinical Isolates to Some Macrolide Antibiotic Groups
DOI:
https://doi.org/10.51173/jt.v5i4.1730Keywords:
Burn Samples, Cefoxitin, D-Phenotype, Erythromycin, MRSAAbstract
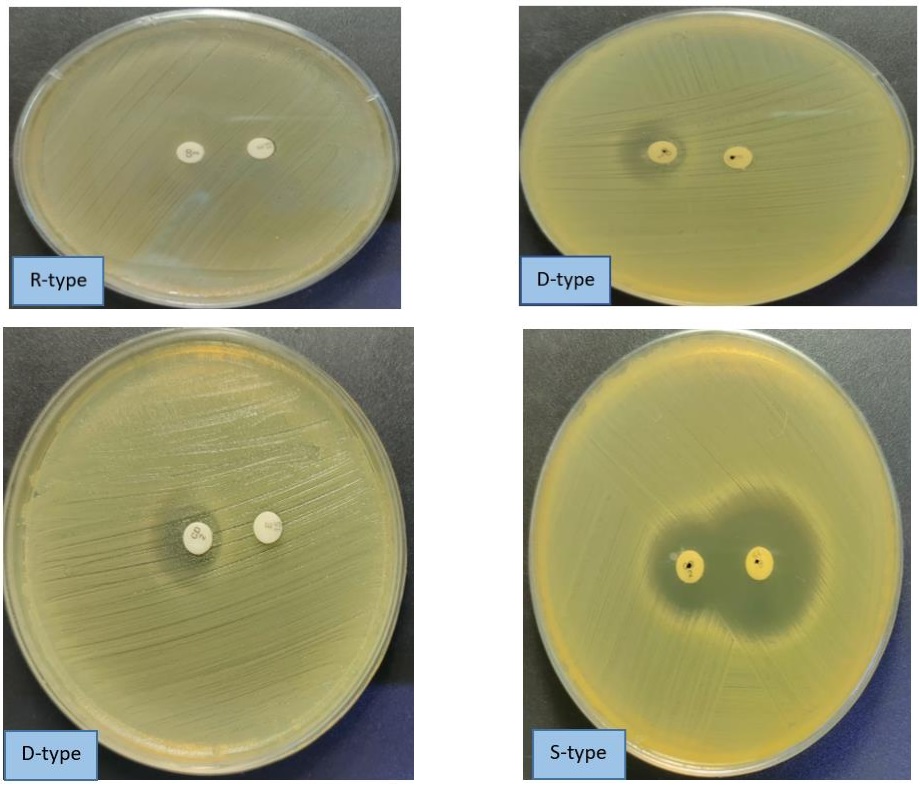
Antimicrobial resistance is one of the most significant global threats to human health in recent times, and it limits the achievement of several of the sustainable development goals. Methicillin-resistant Staphylococcus aureus (MRSA) is among the most essential multidrug-resistant bacterial pathogens. The study aimed to determine the prevalence of (MRSA) from different clinical samples to emphasise the suitable treatment. One hundred fifty different clinical samples were collected. All these samples were subjected to classical microbiological testing, which included culturing directly on mannitol salt agar and antibiotic susceptibility test (A.S.T). The results observed that only 32 out of 150 samples of MRSA isolates were identified using cefoxitin 30 (µg) as a screening antibiotic, as suggested by CLSI. These 32 MRSA isolates showed resistance toward penicillin and cefoxitin, high sensitivity against vancomycin, and moderate resistance against doxycycline and azithromycin. Considering the phenotyping resistance toward macrolide antibiotic groups, 10/32 (31.25%) showed S-phenotype,18/32 (52.65%) showed R-phenotype,4/32 (12.5%) showed D-phenotype while no MRSA isolated showed D+ phenotype. This study concludes that inducible clindamycin resistance of S. aureus (MRSA) increases the difficulty of treating S. aureus bacterial infections.
Downloads
References
S. Reardon, "WHO warns against ‘post-antibiotic era," Nature, vol. 15, pp. 135-8, 2014. https://doi.org/10.1038/nature.2014.15135.
R. E. Duval, M. Grare, and B. Demoré, "Fight against antimicrobial resistance: we always need new antibacterials but for right bacteria," Molecules, vol. 24, no. 17, p. 3152, 2019. doi: 10.3390/molecules24173152.
M. Mišić et al., "Prevalence of genotypes that determine the resistance of staphylococci to macrolides and lincosamides in Serbia," Frontiers in Public Health, vol. 5, p. 200, 2017. doi: 10.3389/fpubh.2017.00200.
D. Oliveira, A. Borges, and M. Simões, "Staphylococcus aureus toxins and their molecular activity in infectious diseases," Toxins, vol. 10, no. 6, p. 252, 2018. DOI: 10.3390/toxins10060252.
K. Kang and S. Redner, "Fluctuation-dominated kinetics in diffusion-controlled reactions," Physical Review A, vol. 32, no. 1, p. 435, 1985. DOI: 10.1103/physreva.32.435.
S. De Backer et al., "Enzymes catalysing the TCA-and urea cycle influence the matrix composition of biofilms formed by methicillin-resistant Staphylococcus aureus USA300," Microorganisms, vol. 6, no. 4, p. 113, 2018. DOI: 10.3390/microorganisms6040113.
A. S. Bishr, S. M. Abdelaziz, I. S. Yahia, M. A. Yassien, N. A. Hassouna, and K. M. Aboshanab, "Association of Macrolide Resistance Genotypes and Synergistic Antibiotic Combinations for Combating Macrolide-Resistant MRSA Recovered from Hospitalized Patients," Biology, vol. 10, no. 7, p. 624, 2021. doi: 10.3390/biology10070624.
G. Mancuso, A. Midiri, E. Gerace, and C. Biondo, "Bacterial antibiotic resistance: The most critical pathogens," Pathogens, vol. 10, no. 10, p. 1310, 2021. DOI 10.3390/pathogens10101310.
G. P. Dinos, "The macrolide antibiotic renaissance," British Journal of Pharmacology, vol. 174, no. 18, pp. 2967-2983, 2017. DOI: 10.1111/bph.13936.
W. Yao et al., "Staphylococcus aureus with an erm-mediated constitutive macrolide-lincosamide-streptogramin B resistance phenotype has reduced susceptibility to the new ketolide, solithromycin," BMC infectious diseases, vol. 19, pp. 1-8, 2019. DOI:10.1186/s12879-019-3779-8.
M. Miklasińska-Majdanik, "Mechanisms of resistance to macrolide antibiotics among Staphylococcus aureus," Antibiotics, vol. 10, no. 11, p. 1406, 2021. doi.org/10.3390/antibiotics10111406.
S. Armin, F. Fallah, M. Navidinia, and S. Vosoghian, "Prevalence of blaOXA-1 and blaDHA-1 AmpC β-lactamase-producing and methicillin-resistant Staphylococcus aureus in Iran," Archives of Pediatric Infectious Diseases, vol. 5, no. 4, 2017. DOI: https://doi.org/10.5812/pedinfect.36778.
E. P. L. Pereira-Franchi, M. R. N. Barreira, N. d. S. L. M. d. Costa, C. M. C. B. Fortaleza, and M. d. L. R. d. S. d. Cunha, "Prevalence of and risk factors associated with the presence of Staphylococcus aureus in the chronic wounds of patients treated in primary health care settings in Brazil," Revista da Sociedade Brasileira de Medicina Tropical, vol. 50, pp. 833-838, 2017. 10.1016/j.bjid.2021.101636.
D. George and P. Mallery, "IBM SPSS Statistics 26 Step by Step A Simple Guide and Reference sixteenth edition," ed: Taylor & Francis, 2020.
C. G. Mayhall, Hospital epidemiology and infection control. Lippincott Williams & Wilkins, 2012.
C. E. Ramirez-Blanco, C. E. Ramirez-Rivero, L. A. Diaz-Martinez, and L. M. Sosa-Avila, "Infection in burn patients in a referral centre in Colombia," Burns, vol. 43, no. 3, pp. 642-653, 2017. DOI: 10.1016/j.burns.2016.07.008.
N. A. Chaudhary et al., "Epidemiology, bacteriological profile, and antibiotic sensitivity pattern of burn wounds in the burn unit of a tertiary care hospital," Cureus, vol. 11, no. 6, 2019. doi: 10.7759/cureus.4794.
M. K. Khudhair and M. A. AlAubydi, "Determination the prevalence and antimicrobial susceptibility of bacteria isolated from burns and wounds," Iraqi Journal of Agricultural Sciences, vol. 54, no. 1, pp. 93-99, 2023. DOI: https://doi.org/10.36103/ijas.v54i1.1679.
E. Ekawati, W. Darmanto, and S. Wahyuningsih, "Detection of Staphylococcus aureus in wound infection on the skin surface," in IOP Conference Series: Earth and Environmental Science, 2020, vol. 456, no. 1: IOP Publishing, p. 012038. DOI 10.1088/1755-1315/456/1/012038.
G. C. M. Almeida, M. M. dos Santos, N. G. M. Lima, T. A. Cidral, M. C. N. Melo, and K. C. Lima, "Prevalence and factors associated with wound colonization by Staphylococcus spp. and Staphylococcus aureus in hospitalized patients in inland northeastern Brazil: a cross-sectional study," BMC infectious diseases, vol. 14, no. 1, pp. 1-8, 2014. DOI: 10.1186/1471-2334-14-328.
W. Norbury, D. N. Herndon, J. Tanksley, M. G. Jeschke, C. C. Finnerty, and S. S. C. o. t. S. I. Society, "Infection in burns," Surgical infections, vol. 17, no. 2, pp. 250-255, 2016. doi: 10.1089/sur.2013.134.
L. Thorlacius-Ussing, H. Sandholdt, A. R. Larsen, A. Petersen, and T. Benfield, "Age-dependent increase in the incidence of Staphylococcus aureus bacteremia, Denmark, 2008–2015," Emerging Infectious Diseases, vol. 25, no. 5, p. 875, 2019. doi: 10.3201/eid2505.181733.
O. E. Akanbi, H. A. Njom, J. Fri, A. C. Otigbu, and A. M. Clarke, "Antimicrobial susceptibility of Staphylococcus aureus isolated from recreational waters and beach sand in Eastern Cape Province of South Africa," International journal of environmental research and public health, vol. 14, no. 9, p. 1001, 2017. DOI: 10.3390/ijerph14091001.
C. A. Bastidas, I. Villacrés-Granda, D. Navarrete, M. Monsalve, M. Coral-Almeida, and S. G. Cifuentes, "Antibiotic susceptibility profile and prevalence of mec A and lukS-PV/lukF-PV genes in Staphylococcus aureus isolated from nasal and pharyngeal sources of medical students in Ecuador," Infection and Drug Resistance, pp. 2553-2560, 2019. doi: 10.2147/IDR.S219358.
J. Fri, H. A. Njom, C. N. Ateba, and R. N. Ndip, "Antibiotic resistance and virulence gene characteristics of methicillin-resistant Staphylococcus aureus (MRSA) isolated from healthy Edible Marine Fish," International journal of microbiology, vol. 2020, 2020. DOI: 10.1155/2020/9803903.
S. S. Khoramrooz et al., "Detection of tetracycline resistance genes, aminoglycoside modifying enzymes, and coagulase gene typing of clinical isolates of Staphylococcus aureus in the Southwest of Iran," Iranian Journal of Basic medical sciences, vol. 20, no. 8, p. 912, 2017. DOI: 10.22038/IJBMS.2017.9114.
S. S. Mahmmod and W. G. AlHadban, "Assessing the prevalence and antibiotic susceptibility patterns of S. aureus bacteria isolated from Iraqi women with vaginosis," Iraqi Journal of Science, vol. 63, no. 10, pp. 4234-4240, 2022. DOI: https://doi.org/10.24996/ijs.2022.63.10.10.
S. M. Hantoosh, "Nasal Carriage of Vancomycin-and Methicillin-Resistant Staphylococcus aureus among Intermediate Students of Urban and Rural Schools of Muthanna Province in Iraq," Iraqi Journal of Pharmaceutical Sciences (P-ISSN 1683-3597 E-ISSN 2521-3512), vol. 31, no. 1, pp. 102-108, 2022. DOI https://doi.org/10.31351/vol31iss1pp102-108.
R. Timsina, U. Shrestha, A. Singh, and B. Timalsina, "Inducible clindamycin resistance and erm genes in Staphylococcus aureus in school children in Kathmandu, Nepal," Future Science OA, vol. 7, no. 1, p. FSO361, 2020. DOI: 10.2144/from-2020-0092.
S. H. Aubaid, E. S. Falih, and S. Khalid Ibrahim, "Biofilm Formation of Staphylococcus Aureus in Multiple Sclerosis Patients and its Essential Role in the Pathogenicity of the Disease," Journal of Techniques, vol. 4, no. 3, pp. 14-18, 2022. DOI: https://doi.org/10.51173/jt.v4i3.511.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Ali Yaseen, Jaleel Samanje, Qahtan Adnan Rasheed, Rafah Sabah Barrak, Afraa Brahim

This work is licensed under a Creative Commons Attribution 4.0 International License.